Introduction
More than 85% of post-stroke patients experience impaired upper limb functionality on the hemiplegic side [1]. In general, 55%-75% of the sequelae remain even three to six months later [2].
Furthermore, coordination of both sides of the upper extremity is
needed to accomplish most daily activities such as face washing, tooth
brushing, eating, and getting dressed [1].
Therefore, assisting individuals with stroke in recovering the use of
their affected upper limbs was a crucial goal for rehabilitation.
Recently, sensory stimulation has often been applied simultaneously
with motor stimulation in stroke-affected limbs. Sensory stimulation
techniques, such as transcutaneous electrical nerve stimulation (TENS) [3-8] and thermal stimulation (TS) [9-11]
have demonstrated more favorable effects on motor recovery or pain
relief than motor training alone for post-stroke survivors. TENS
intervention on the lower extremity demonstrated significant positive
effects on the decrease in the hyperactivity stretch reflex, maximal
voluntary contraction of the ankle dorsiflexor [12], and walking speed [13]
in individuals with chronic stroke. Furthermore, the effects of
combining TENS with task-oriented interventions showed significantly
greater improvement in motor function and spasticity compared to
task-oriented interventions alone for individuals with chronic stroke [5].
Hence, TENS interventions for chronic stroke may positively affect
motor recovery or spasticity. On the other hand, TS, which is a sensory
stimulation intervention, is usually used with hot and cold packs
wrapped in the target region, and TS intervention demonstrated a
significant increase in motor function and Brunnstrom stage for
individuals with acute stroke [11], subacute stroke [14], and chronic stroke [15].
A possible explanation for the effectiveness of TS on sensory and
motor function improvements might be that, during the acute phase of
stroke, the cerebral cortex undergoes regrouping [16,17].
This constitutes a timely opportunity for the application of high
levels of sensory stimulation to the affected limbs for the activation
of specific cortical areas, thereby improving sensory and motor
functions and alleviating secondary injuries caused by the loss of those
functions [18].
Hence, the application of sensory stimulation to improve motor function
in patients with stroke should be addressed in the rehabilitation
protocol. Clinically, both TENS and TS are easily used and applied as
rehabilitation approaches, and both interventions facilitate motor
function restoration owing to the stimulation of peripheral sensory
receptors and further cause excitation of the cortex [15].
Thus, investigations on the effects of TS, TENS, and conventional
therapy on motor recovery of the upper extremities are essential to
provide evidence for therapists to choose rehabilitation approaches and
protocols. However, few studies have used sensory stimulation
accompanied by motor training in stroke patients during the acute phase
to determine their effects. Thus, the present study aimed to investigate
the effects of TENS and TS combined with motor training on sensory and
motor recovery in the upper extremities of patients with acute stroke.
This study hypothesized that sensory stimulation might improve sensory
and motor functions in individuals with acute stroke.
Materials & Methods
Trial design
This is a parallel study design; patients with acute stroke were
assigned to the TS group, TENS group, or control group using a random
number drawing method by the investigator. Assessment of sensory and
motor recovery of the upper limb was performed the day before and the
day after the intervention. The assessments were performed by the
investigator, while the intervention was performed by two
physiotherapists familiar with the research procedures. The study
protocol was approved by the institutional review board of E-Da Hospital
(approval number EMRP-103-113) and was registered on the ISRCTN
registry (no. ISRCTN62945682). This study is a non-blinding design. One
experienced physical therapist performed the intervention and the
evaluation for all participants. The experiment was conducted in E-Da
Hospital, Kaohsiung, Taiwan.
Participants
The sample size of this study was evaluated by power analysis using
G*Power Ver.3.1.9.2 (Heinrich-Heine-Universität Düsseldorf, Düsseldorf,
Germany). The power analysis results revealed that a minimum sample size
of 25 participants was required in this study with a significance level
of 0.05, and statistical power of 0.8 for an analysis of covariance
(ANCOVA) design.
Thirty participants were randomly assigned to one of three groups (n =
10 each): the TS, TENS, and control groups. The participants were
inpatients with stroke at the E-Da Hospital. Patients who (1) were aged
20 years or older; (2) had a stroke for the first time and exhibited
hemiparesis; (3) were hospitalized during the acute phase; (4) did not
have obvious cognitive impairments; (5) could independently maintain a
sitting posture for at least 30 min; and (6) had provided written
informed consent for participation in this study were included. Patients
were excluded if they (1) had skin conditions or injuries (e.g.,
wounds) on their upper limbs or had other contraindications for
electrotherapy or TS (e.g., a malignant tumor); (2) had a language
disorder (e.g., aphasia) and were therefore unable to communicate or
comply with instructions; (3) had other orthopedic conditions (e.g.,
severe arthritis) or nerve damage (e.g., peripheral nerve injury)
affecting movement in their upper limbs; (4) had diabetes or complete
sensory impairment not caused by stroke (e.g., peripheral vascular
disease or neuropathy); (5) had developed neurological disorders during
the experimental period or other conditions that may have affected the
study results; (6) had uncontrolled hypertension, unstable angina, a
history of myocardial infarction, epilepsy (except for febrile seizures)
in the past three months, or a pacemaker; or (7) had participated in
other rehabilitation or drug trials. One participant from both the TS
and TENS groups withdrew from the study after discharge from the
hospital, and one participant in the control group withdrew due to poor
attendance. Thus, nine participants remained in each of the three groups
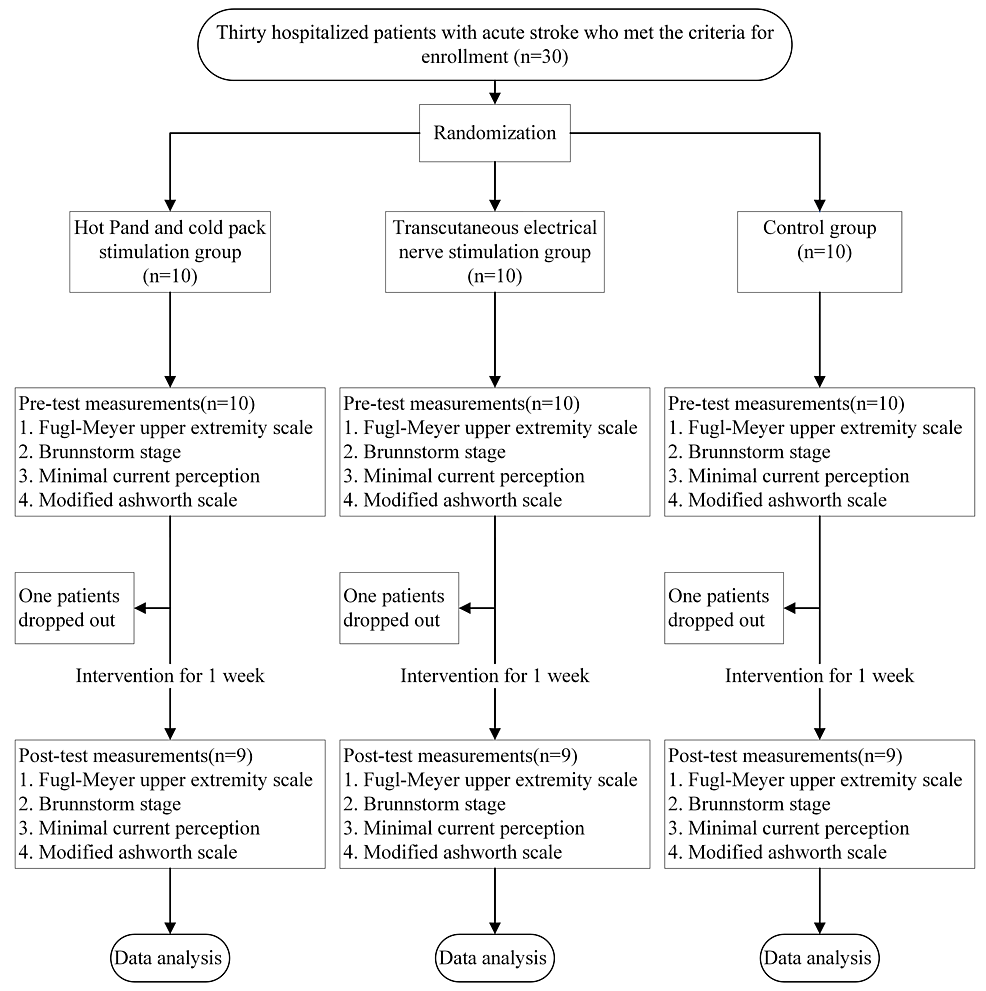
(total, n=27). The experimental flowchart is shown in Figure 1.
Treatment sessions
TS Group
In the TS group, the following equipment and intervention protocol
were used. The hot and cold stimulation devices used were a Firstek
heating circulator water bath (B300, Firstek Corp, Taiwan) and a Firstek
cooling circulator water bath (B401L, Firstek Corp, Taiwan),
respectively. Each was connected to a temperature therapy pad (TP22E,
Gaymer Corp, USA). For the hot and cold stimulation, the temperatures
were set at 51°C and 4°C, respectively. The participants received hot
and cold stimulation in 30-minute sessions administered twice daily
(once in the morning and afternoon, respectively) over five days,
totaling 10 sessions. In accordance with the procedure used in one study
[10],
participants receiving TS were instructed to sit with both hands flat
on the table. Heat stimulation was applied to their healthy arm for no
more than 15 minutes. A thermometer was placed on the stimulated body
part to prevent frostbite or burns. The therapy pad was wrapped around
the palm and wrist of the affected limb. During the session, the
therapist encouraged the participants to pull their limbs from the
therapy pad through active movements. They were instructed to remove
their healthy hand when they began feeling discomfort or when a score of
seven had been reached on a standard 10-point visual analog scale
(administered by the therapist), and the time from the beginning of the
session to this point was recorded. The same procedure was repeated with
the participants’ affected forearm. If no adverse skin reactions
occurred, heat was applied on their affected arm 10 consecutive times,
separated by three minutes of rest. Cold therapy involved the same
procedure and was applied alternately with heat therapy. With both heat
and cold therapy, TS was applied for 15 seconds, followed by at least 30
seconds of rest. Heat and cold were applied 20 times in each session.
During each session, the therapist constantly measured the skin surface
temperature on the tested limb to prevent frostbite or burns.
TENS Group
Portable TENS (TRIO-310, ITO, Japan) was used for the intervention in
the TENS group. The patches were adhered to the forearm. The skin was
cleaned with alcohol before and after each disinfection session to
reduce the possibility of increased electrical resistance. Wounds were
avoided during the study. The TENS settings were as follows: pulse
width, 200 µs; output frequency, 100 Hz; output time, 30 minutes. The
output frequency was selected mainly for stimulating the Aβ fibers,
which produce sensations of light touch and pressure [19].
The current strength was adjusted to the maximum that participants
could withstand. As with TS, TENS was applied in 30-minute session
administered twice daily (once in the morning and afternoon) over five
days, totaling 10 sessions. Moreover, the therapist monitored the
participants during each session and measured their blood pressure,
heart rate, and breathing before and after the intervention, adjusting
the rest periods as necessary and taking care to prevent electrical
burns.
Control Group
Participants in the control group received regularly scheduled
rehabilitation therapy (one hour each of physical and occupational
therapy). Physical therapy includes therapeutic exercise, facilitation
training, and functional training. Occupational therapy involves hand
function training for activities of daily living.
Outcome measurements
Outcome measures were conducted before and after a one-week
intervention. The Fugl-Meyer Upper Extremity (FMUE) scale, Brunnstrom
stage classification-proximal and distal ends of the upper limb, minimal
current perception (MCP), and modified Ashworth scale (MAS) for the
elbow flexor and wrist flexor were used to evaluate the intervention
effects.
FMUE Scale Assessment
FMUE measurements were used to evaluate motor function, sensory
function, joint range of motion, and balance. An ordinal level of
measurement was used. The FMUE has high reliability (intraclass
correlation coefficient, ICC=0.99) for evaluating motor function after
post-stroke [20].
Brunnstrom Stage Assessment
Brunnstrom stage was used to evaluate motor recovery after brain
injury. There were six evaluation stages. Stage 1 is flaccid, which
means that the limb does not have movement or muscle tone, while stage 6
is near normal, which means that the motor performance of the limb is
near normal. The Brunnstrom stage classification had high intra- and
inter-rater reliability (ICC for inter-rater=0.94, ICC for
intra-rater=0.97) [21].
Minimal Current Perception
Pain vision PS-2100 (Nipro Co., Osaka, Japan) was used to evaluate
sensory deficits in individuals with stroke. The electrical stimulation
frequency was set at 50 Hz. Participants held a switch on the device to
activate and stop the device. The weak current increased gradually when
the participant switched on the device. The participant was then asked
to switch off the device when they felt the current [22].
MAS Assessment
This study evaluated the spasticity of the elbow and wrist flexors
using MAS. MAS is a reliable assessment tool for evaluating limb
spasticity (ICC=0.86) [23].
First, the joint range of motion was measured, and the therapist
manually stretched the participants to observe limb resistance.
Statistical analysis
Analyses were conducted using IBM SPSS Statistics for Windows,
version 20.0 (IBM Corp., Armonk, NY, USA). Chi-square tests were
performed on categorical variables to determine the presence of
between-group differences based on sex, affected side, and stroke type.
Continuous demographic data and baseline measurements were evaluated
using a one-way analysis of variance (ANOVA).
One-way analysis of covariance (ANCOVA) and paired t-tests were
performed to determine between-group differences and significant
differences between the pre-test and post-test in each group. The
significance level was set at p<0.05. The Bonferroni correction was
used for post-hoc comparisons.
Results
The three groups showed no significant differences in the demographic data and baseline outcome measurements (Table 1).
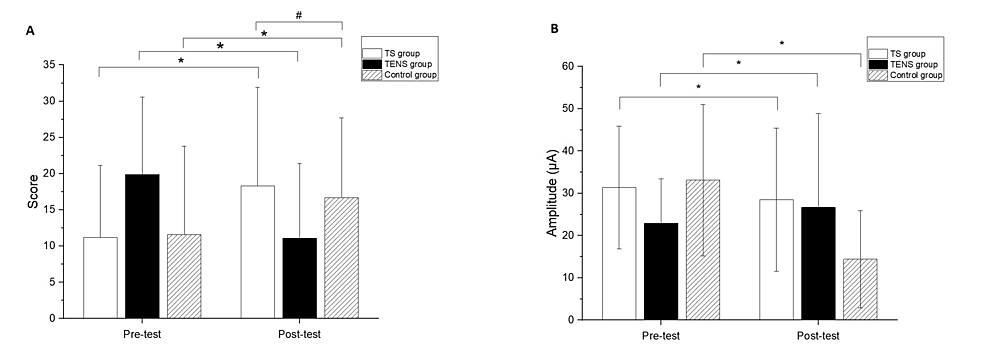
Significant differences after the intervention compared to baseline
measurements were found in the FMUE for all groups (TS group, 95% CI:
-10.00, -7.34, p<0.01; TENS group, 95% CI: -8.15 and -5.40,
p<0.01; control group, 95%CI: -7.77 and -3.34, p<0.01) (Figure 2A). In addition, a significant difference between the TS and control groups was observed in the FMUE (p=0.02) (Figure 2A).
The comparisons of the differences of pre- and post-test were
significant in MCP for all groups (TS group, 95%CI:2.48 and 14.92,
p=0.02; TENS group, 95% CI:1.37 and 7.81, p=0.01; control group, 95%
CI:1.15 and 7.78, p=0.01) (Figure 2B). However, there were no significant differences among the groups at the post-test in the MCP test.
Significant differences were found in the FMUE for all groups
compared to baseline measurements (TS group, 95% CI: -10.00, -7.34,
p<0.01; TENS group, 95% CI: -8.15 and -5.40, p<0.01; control
group, 95%CI: -7.77 and -3.34, p<0.01), with a significant difference
observed between the TS and control groups (p=0.02). Additionally,
significant differences in MCP were found in all groups comparing pre-
and post-test values (TS group, 95%CI: 2.48 and 14.92, p=0.02; TENS
group, 95% CI: 1.37 and 7.81, p=0.01; control group, 95% CI: 1.15 and
7.78, p=0.01) (Figures 2A, 2B). However, no significant differences among the groups were observed in the post-test in the MCP test.
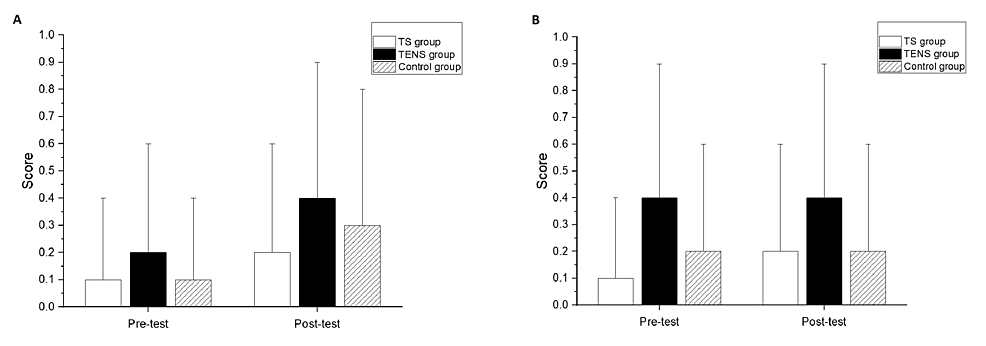
Significant differences after the intervention compared to the
baseline measurements were not found in the MAS of the elbow flexors for
all groups (Figure 3A) or the wrist flexors for all groups (Figure 3B).
There were no significant differences among the groups at post-test in
the MAS scores of the elbow flexors and wrist flexors (Figures 3A, 3B).
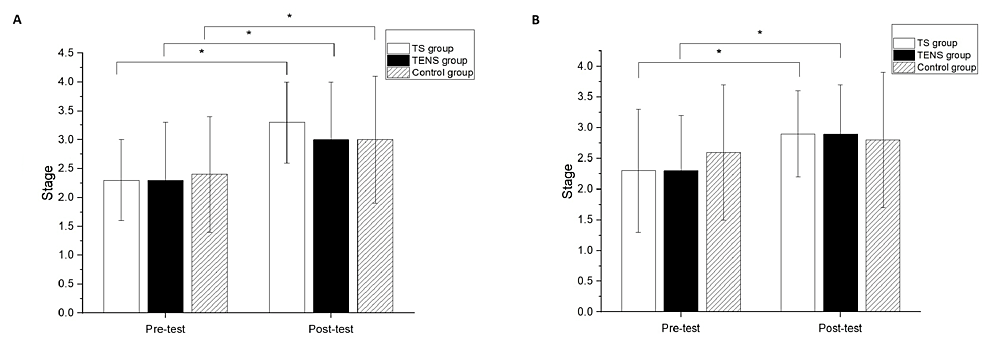
Significant differences after the intervention compared to baseline
measurements were found in the Brunnstrom stage classification of the
proximal end for all groups (TS group, p<0.01; TENS group, p<0.01;
control group, p=0.02) (Figure 4A).
However, there was no significant difference among the groups in the
Brunnstrom stage classification of the proximal end at the post-test
(Figure 4A).
Significant differences after the intervention compared to the baseline
measurements were found in the Brunnstrom stage classification of the
distal end for the TS group (p=0.02) and the TENS group (p=0.04) (Figure
4B);
however, there was no significant difference between the pre-test and
post-test in the Brunnstrom stage classification of the distal end for
the control group. There was no significant difference among the groups
in the Brunnstrom stage classification of the distal end at the
post-test (Figure 4B).
Discussion
In the current study, TS and TENS interventions were applied for one
week to evaluate their effects on the recovery of motor and sensory
functions in the upper limbs of acute stroke patients. Significant
improvements in FMUE scores were observed in all three groups after the
intervention, with the TS group showing superior performance compared to
the control group. Short-term improvements in motor function, with no
differences in spasticity in the elbow and wrist flexors, were seen in
all groups according to MCP results. The proximal end of the Brunnstrom
stage showed significant short-term improvements in all groups, while
the distal end showed immediate improvement only in the experimental
group after one week. These results suggest the efficacy of TS and TENS
in improving short-term motor recovery in acute stroke patients.
Additionally, the study highlighted the significant effects of the TS
intervention on FMUE, supporting its role as a sensory stimulation tool
in restoring motor function during stroke recovery. Previous research
has further supported the positive effects of TS on motor recovery in
acute and subacute stroke patients, as observed on the Action Research
Arm Test and the upper extremity subscale of the Stroke Rehabilitation
Assessment of Movement [9,11].
TS and TENS have shown promise in managing acute stroke patients.
Previous research has shown that repetitive sensory stimulation and mass
motor practice could promote neuroplasticity and cortical
reorganization in stroke patients, which might contribute to improved
motor function [6].
There was also evidence indicating that TENS had demonstrated positive
outcomes in alleviating brain damage following ischemic stroke by
reducing oxidative stress, inhibiting neuronal pyroptosis, and
activating mitophagy pathways [24]. Therefore,
both TS and TENS, either individually or in combination, could be
valuable adjuncts to conventional therapy in enhancing motor recovery
and functional outcomes in acute stroke patients.
With our understanding, this study was the first to compare the
recovery of motor and sensory functions in the upper limbs of
individuals with acute stroke by simultaneously applying TS and TENS,
common modalities in clinical rehabilitation [6,24].
Several studies have suggested the benefits of both TS and TENS for
motor recovery in acute stroke patients. However, most of these studies
had focused on either one modality or a combination with other
interventions, such as TENS with taping [25].
Nevertheless, there has been little research comparing the efficacy of
TS and TENS concurrently for upper limb motor recovery in individuals
with acute stroke.
Between-group comparisons revealed that the TS group demonstrated
more substantial post-intervention improvements in terms of the FMUE
scores than the control group. In contrast, the TENS group did not
significantly outperform the control group. Notably, all three groups
exhibited significant improvements in the FMUE scores in the post-test,
with the TS group outperforming the control group. The higher
performance of the TS group on the FMUE scores compared to the other
groups might be due to several factors. First, many of the items
assessed in the FMUE were related to distal hand and wrist control,
which correlated with improvements in the distal Brunnstrom stage.
Another possible reason might have been the active participation in the
thermal and cold stimulation procedure, which involved moving the hand
back and forth, which was believed to enhance proprioceptive input,
leading to improved motor control in the affected upper limb movements [26].
This suggests that motor learning potentially boosts proprioception and
body movements by influencing the relationship between somatosensory
and motor systems through neural pathways. This active participation
likely contributed to the improvement in FMUE scores. In contrast, the
TENS group largely maintained a static posture during the intervention,
resulting in no significant difference in FMUE improvement compared to
the control group.
The TENS group also exhibited significant improvements after the
intervention, but these changes were not significant compared with the
control group. This result does not support the premise that the motor
improvements observed in the TENS group were attributable to the
intervention. The previous study involved individuals in the chronic
phase of stroke who received a combination of upper extremity TENS and
task-related training (30 minutes per day, five days per week, four
weeks). This intervention resulted in significant improvements in a
variety of assessments, including the FMUE, the Manual Functional Test,
the Box and Block Test, and the MAS. Specifically, the group that
received TENS in addition to task-oriented training showed significant
improvement, particularly in reducing spasticity according to the MAS.
In contrast, the control group, which received placebo TENS and
task-oriented training, did not show similar improvement. The
researchers concluded that the improved motor function was primarily due
to motor training effects and highlighted the effectiveness of TENS in
reducing spasticity [27].
In the present study, the spasticity scores on the MAS of 0.2±0.4
indicated low tension, which is understandable given that the
participants were all in the acute phase. This also explains why the
effects of TENS were less apparent.
Overall, all three groups demonstrated improvements in motor function
after the intervention. This may be associated with the fact that the
participants were in the acute phase when brain reorganization was the
most active. Although this result was only observed in the FMUE group,
significant post-intervention differences were only present between the
TS and control groups. Less substantial differences were noted between
the TENS and control groups; however, based on the mean value, the TENS
group improved more than the control group. Moreover, the proximal and
distal parts of the Brunnstrom stage indicated that both TS and TENS
resulted in greater improvement. Therefore, it could be suggested that
additional interventions using TS or TENS could potentially aid in the
recovery of upper limb motor function in individuals with acute stroke.
This research was in line with findings from previous studies, which
suggested that TS and TENS activated the cortical areas responsible for
motor function [5,28].
Regarding the assessment of sensory function, the present study used
devices that allowed for the quantification of perception and pain with
regard to the MCP of each participant. In all three groups, the
postintervention MCP differed significantly from the preintervention
MCP; however, no significant between-group differences were observed. A
study reported that individuals with stroke (three months after stroke
occurrence) who received intermittent pneumatic compression (30-min
sessions, five days a week, four weeks) with conventional rehabilitation
treatments outperformed the control group, who only received
conventional rehabilitation treatments on the Nottingham Sensory
Assessment Scale, two-point discrimination test, and tactile and joint
kinesthesia assessments, despite both groups demonstrating significant
post-intervention improvements [29].
In a similar study, the experimental and control groups underwent TS
(sessions of 20-30 min, five days a week, six weeks) and conventional
rehabilitation, respectively. Both groups had significant
post-intervention improvements in the Semmes-Weinstein monofilament
test, with the experimental group outperforming the control group [11].
These collective results suggest that interventions during the acute
phase of stroke can lead to considerable improvements in the recovery of
sensory function regardless of the use of additional sensory inputs.
Moreover, sensory stimulation appears to exert more substantial benefits
on sensory recovery than conventional rehabilitation. Furthermore,
although significant improvements were observed among all three groups
after the intervention, no significant between-group differences were
detected. This might be because the intervention lasted only one week,
which was considerably shorter than that in previous studies (at least
four weeks).
In the present study, the MAS measurements of the elbow and wrist
flexors did not change significantly after the intervention in any
group. A previous study applied TENS to the upper limbs of individuals
with stroke (on average, 12 months post-stroke). The intervention
comprised 30-min sessions administered five times a week over four
weeks, and similarly, the stroke individuals exhibited a significant
reduction in muscle tension after the intervention [5].
The following arguments regarding the mechanism by which TENS reduces
post-stroke spasticity have been proposed. First, TENS can promote the
release of the inhibitory neurotransmitter gamma-aminobutyric acid in
the posterior gray column [30].
Second, spasticity is caused by hyperexcitability of the central
nervous system. The application of TENS to the surrounding nerves can
lower spasticity through reciprocal inhibition [5].
In the present study, no changes in spasticity or significant
differences were observed among the three groups after the intervention.
This may be because the intervention period of five days was not
sufficient to induce a significant reduction in spasticity.
Study limitations
There were some limitations in interpreting the results of this
study. First, the intervention period of this study was only five days;
hence, it may not be sufficient to improve spasticity. Second, the
sample size was relatively small; there were only nine participants with
acute stroke in each group. Finally, this study had a non-blinded
design, which may have influenced the results. Second, this study had a
non-blinded design; one experienced physical therapist carried out the
evaluation and intervention, while the study did not include the placebo
group; hence, the participants were not blinded.
Conclusions
The use of TS in individuals with acute stroke demonstrated a
significant improvement in pain perception compared to conventional
physical therapy. Both TS and TENS had positive effects on motor
function recovery at the distal end of the upper limb compared with
baseline measurements. This study suggested that incorporating TS or
TENS in the rehabilitation protocol potentially improved motor function
in individuals with acute stroke, compared to those who received
conventional physical therapy alone.